Intro
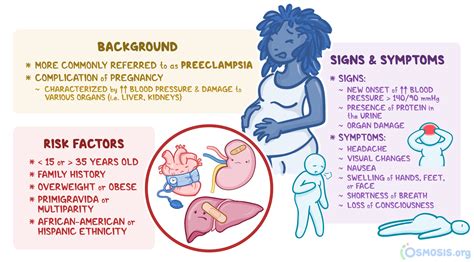
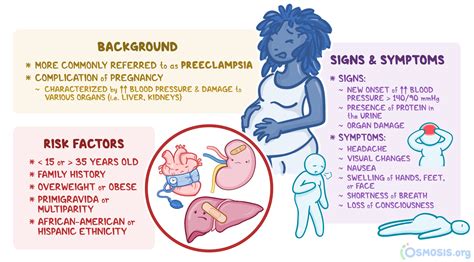
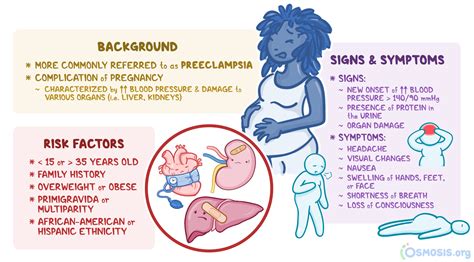
The postpartum period is a critical and vulnerable time for new mothers, marked by significant physical, emotional, and hormonal changes. Among the various complications that can arise during this period, postpartum toxemia, also known as postpartum preeclampsia or postpartum eclampsia, is a condition that requires immediate medical attention. Understanding the symptoms of postpartum toxemia is essential for early detection and intervention, which can significantly improve outcomes for both the mother and the baby.
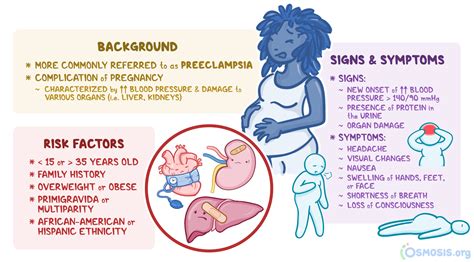
Postpartum toxemia is a condition characterized by the onset of high blood pressure and often accompanied by significant amounts of protein in the urine, occurring after childbirth. This condition can lead to more severe complications, including seizures (eclampsia), stroke, and even death if not promptly treated. The risk factors for developing postpartum toxemia include a history of preeclampsia during pregnancy, chronic hypertension, pre-existing kidney or liver disease, and certain obstetric complications.
The importance of recognizing the symptoms of postpartum toxemia cannot be overstated. Early detection allows for timely medical intervention, which can prevent the progression to more severe forms of the disease. Moreover, awareness of these symptoms can empower new mothers and their families to seek medical help promptly, potentially saving lives. The symptoms of postpartum toxemia can be subtle and may resemble those of other less severe conditions, making it crucial for healthcare providers to be vigilant and for patients to be aware of their bodies' signals.
Introduction to Postpartum Toxemia
Postpartum toxemia is a multifactorial condition, and its exact causes are still under research. However, it is believed to result from the body's response to the sudden changes post-delivery, including the release of certain factors from the placenta that can affect blood vessel function and blood pressure regulation. Understanding the pathophysiology of postpartum toxemia is key to developing effective prevention and treatment strategies.
Pathophysiology of Postpartum Toxemia
The pathophysiology involves complex interactions between the vascular endothelium, the coagulation system, and inflammatory responses. These interactions can lead to endothelial dysfunction, increased vascular resistance, and the clinical manifestations of hypertension and proteinuria. The condition can also affect other organ systems, including the kidneys, liver, brain, and clotting system, leading to a wide range of symptoms and potential complications.Symptoms of Postpartum Toxemia
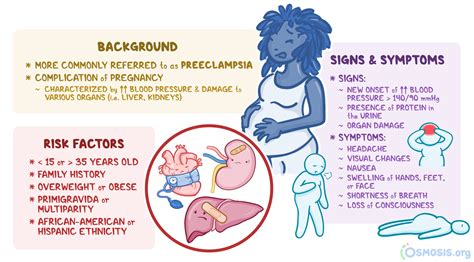
The symptoms of postpartum toxemia can vary in severity and may include:
- High blood pressure: This is often the first sign, and it can be significantly higher than the woman's usual blood pressure.
- Proteinuria: The presence of excessive protein in the urine, which can be detected through urinalysis.
- Severe headache: Not relieved by usual pain medications and can be indicative of increased intracranial pressure.
- Vision changes: Including blurred vision, double vision, or sensitivity to light, which can result from the effect of high blood pressure on the retina.
- Nausea and vomiting: These symptoms can be severe and may lead to dehydration if not managed properly.
- Abdominal pain: Upper abdominal pain, particularly in the right upper quadrant, can be a sign of liver involvement.
- Decreased urine output: As the kidneys are affected, leading to a decrease in urine production.
- Seizures: In the case of eclampsia, which is a severe complication of postpartum toxemia.
Risk Factors for Postpartum Toxemia
Several factors can increase a woman's risk of developing postpartum toxemia. These include: - History of preeclampsia during pregnancy - Pre-existing hypertension or kidney disease - Family history of preeclampsia - Obesity - Multiple gestation (carrying twins or more) - History of certain medical conditions, such as autoimmune diseases or thrombophiliasDiagnosis of Postpartum Toxemia
Diagnosing postpartum toxemia involves a combination of clinical evaluation, laboratory tests, and sometimes imaging studies. The diagnosis is typically made based on the new onset of hypertension and proteinuria after delivery, in the absence of other causes. Blood tests may be performed to assess liver and kidney function, and to check for signs of coagulopathy. Urine analysis is crucial for detecting proteinuria, and a 24-hour urine collection may be necessary for quantification.
Treatment of Postpartum Toxemia
The treatment of postpartum toxemia aims to control blood pressure, prevent seizures, and manage any complications that may arise. This can involve: - Antihypertensive medications to lower blood pressure - Corticosteroids to promote fetal lung maturity if delivery is premature - Magnesium sulfate to prevent seizures - Bed rest, although its effectiveness is debated - Close monitoring of blood pressure, urine output, and for signs of complicationsComplications of Postpartum Toxemia
If left untreated, postpartum toxemia can lead to severe complications, including:
- Eclampsia: The onset of seizures in a woman with preeclampsia
- Stroke: Due to severely elevated blood pressure
- Pulmonary edema: Fluid accumulation in the lungs
- Acute kidney injury: Leading to a decrease in kidney function
- Liver rupture: A rare but potentially life-threatening complication
- Coagulopathy: Disruption of blood clotting mechanisms, leading to an increased risk of bleeding or thrombosis
Prevention Strategies
While postpartum toxemia cannot be entirely prevented, certain strategies can reduce the risk: - Close monitoring of blood pressure and urine protein levels postpartum - Early recognition and management of hypertension - Avoiding postpartum non-steroidal anti-inflammatory drugs (NSAIDs) if at high risk - Considering low-dose aspirin in high-risk women during pregnancyLong-term Implications
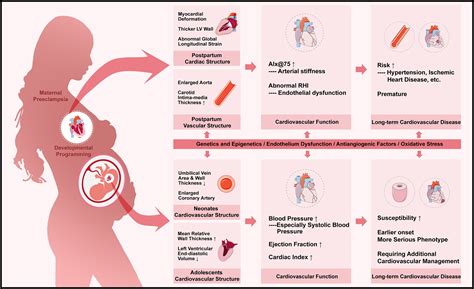
Women who experience postpartum toxemia are at an increased risk of future cardiovascular disease, including hypertension, heart disease, and stroke. Therefore, long-term follow-up with a healthcare provider is essential to monitor for these potential complications and to implement preventive measures.
Support and Resources
New mothers experiencing postpartum toxemia may require significant support, both physically and emotionally. This can include: - Close family and friend support networks - Professional counseling for anxiety or depression - Education on the condition, its management, and potential long-term implications - Access to healthcare services for ongoing monitoring and careConclusion and Future Directions
In conclusion, postpartum toxemia is a serious condition that requires prompt recognition and treatment to prevent severe complications. Continued research into its pathophysiology and risk factors will be crucial for developing effective prevention and management strategies. Raising awareness among healthcare providers and the general public about the symptoms and risks of postpartum toxemia is essential for improving outcomes.
As we move forward, it is critical to prioritize the health and well-being of new mothers, ensuring they receive comprehensive care that addresses both their physical and emotional needs. By working together, we can reduce the incidence and impact of postpartum toxemia, ultimately saving lives and promoting healthier families.
We invite you to share your thoughts, experiences, or questions regarding postpartum toxemia in the comments below. Your engagement can help raise awareness and support for those affected by this condition. Additionally, consider sharing this article with others who may benefit from this information, contributing to a broader understanding and discussion about postpartum health.
What are the primary symptoms of postpartum toxemia?
+The primary symptoms include high blood pressure, proteinuria, severe headache, vision changes, nausea and vomiting, and abdominal pain.
How is postpartum toxemia diagnosed?
+Diagnosis is based on the new onset of hypertension and proteinuria after delivery, confirmed through clinical evaluation, laboratory tests, and sometimes imaging studies.
What are the potential long-term implications of postpartum toxemia?
+Women who experience postpartum toxemia are at an increased risk of future cardiovascular disease, including hypertension, heart disease, and stroke.
